Diabetic Retinopathy
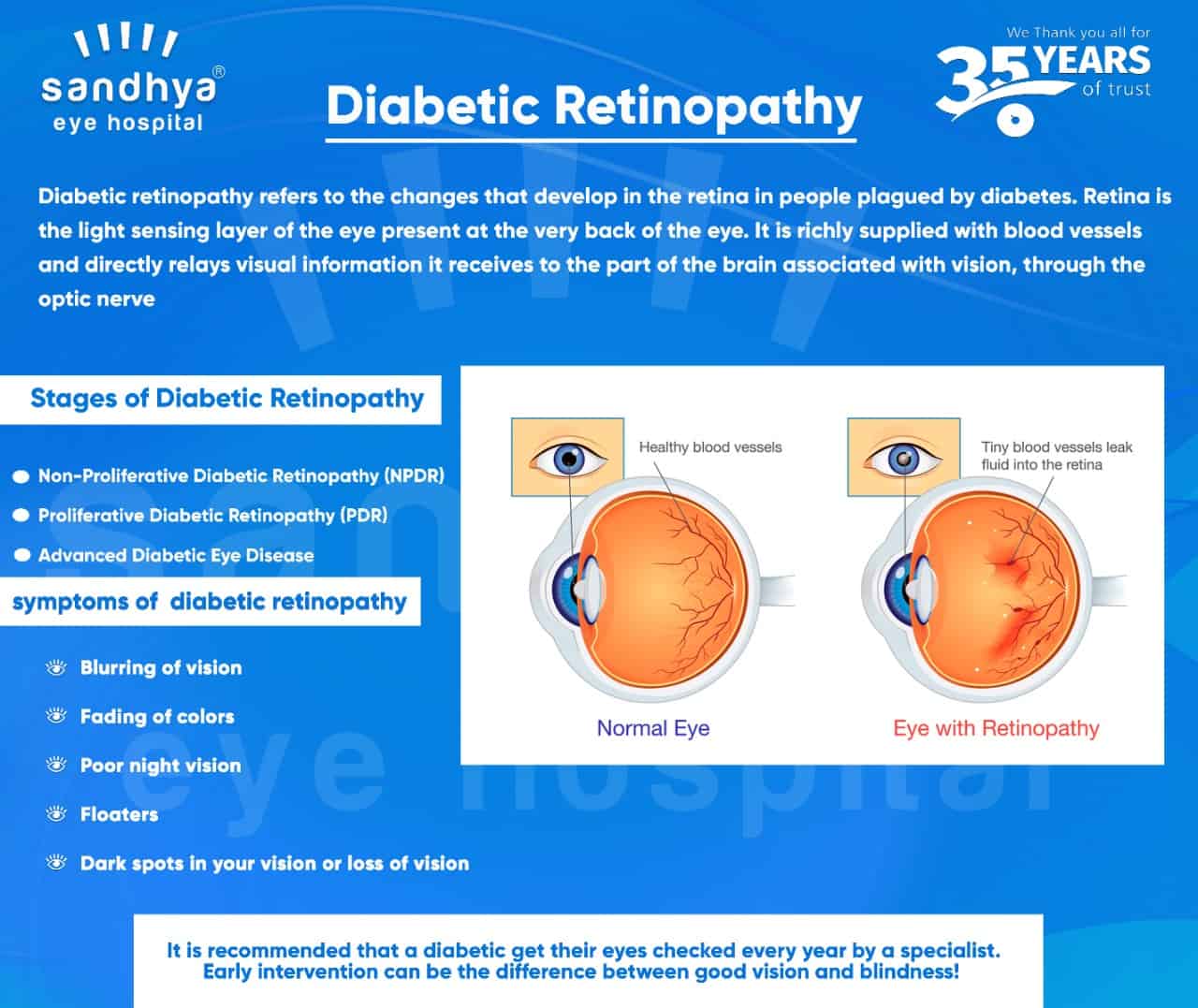
Diabetic retinopathy refers to the changes that develop in the retina in people plagued by diabetes. The retina is the light-sensing layer of the eye present at the very back of the eye. It is richly supplied with blood vessels and directly relays visual information it receives to the part of the brain associated with vision, through the optic nerve. With the increase in life expectancy of people suffering from diabetes more cases of Diabetic retinopathy (DR) is being diagnosed. It has come to such an extent that it is the leading cause of blindness in the developed world!
The duration of diabetes is the most important factor in the development of such a condition with about 20% of diabetics developing DR after 10 years and that number dangerously increasing anywhere between 75% to 90% after 20 years. Heredity, smoking, and poor blood sugar control can accelerate the disease. Other co-morbid diseases like high blood pressure and obesity also accentuate the development of the condition.
The disease develops due to increased blood sugar in the body which damages blood vessels throughout the body by weakening the walls of the vessels. Thus these vessels start leaking blood into the retina causing deterioration of vision.
Symptoms of diabetic retinopathy:
- Blurring of vision
- Fading of colors
- Poor night vision
- Floaters (random spots that float in and out of your vision)
- Dark spots in your vision or loss of vision in particular areas of your sight
Stages of diabetic retinopathy:
- Non-Proliferative Diabetic Retinopathy (NPDR)
NPDR is the earliest stage. It is usually symptomless but can cause a slight blurring of vision. The blood vessels in the retina start leaking blood, causing a range of problems from swelling in a region called macula ( the most sensitive part of the retina), deposits of blood across the retina called hemorrhages, or even ischemia (lack of oxygen) which causes damage to the retina.
- Proliferative Diabetic Retinopathy (PDR)
PDR is the advanced stage and develops in 50% of cases after 25 years. The leaking blood vessels cause a deficiency of blood reaching the retina, and the body reacts by developing new vessels. The problem with such a reaction is that these new vessels leak blood into the vitreous, the substance that makes up nearly 80% of your eye. This can cause floaters in your vision. Scarring of the retina is also common in this stage and that can lead to retinal detachment. PDR is dangerous and can lead to central and peripheral loss of vision.
- Advanced Diabetic Eye Disease
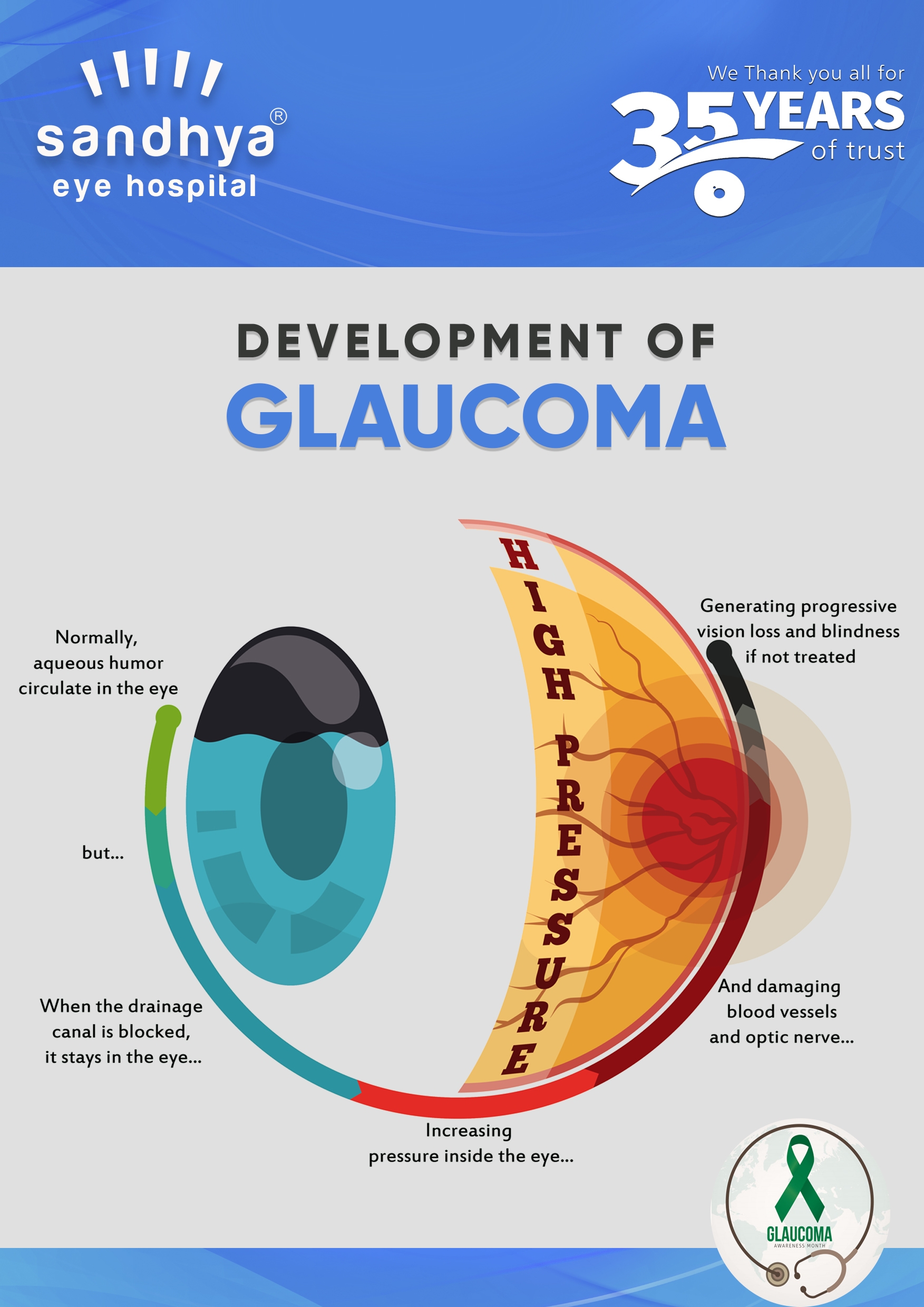
Prolonged diabetic changes in the eye can lead to drastic and dreaded consequences like retinal detachment, vitreous hemorrhage, and glaucoma.
Your doctor will check your blood sugar and perform certain eye tests during a comprehensive eye examination to detect such changes including a slit lamp examination, retinoscopy, and advanced scans called fundus fluorescein angiography.
Treatment of these changes depends on the stage of the disease among other factors and includes:
- Regular eye checkups initially to monitor the development of the disease.
- Injections called anti-VEGF to slow down the changes.
- Laser treatment to plug the leaking blood vessels.
- In advanced cases with scarring, they might recommend a surgery called a vitrectomy.
Screening of diabetics becomes important to detect these changes early and take necessary steps to prevent further damage. It is recommended that a diabetic get their eyes checked every year by a specialist. Early intervention can be the difference between good vision and blindness!